By A. Frillock. Biola University. 2018.
This goal may be expanded edge and skill discount elimite 30 gm visa, and when their behavior does not re- to include helping the person achieve an optimal veal unnecessary trauma as a consequence of illness level of balance and functioning when this is possi- (Johnson 1980 purchase elimite 30gm without prescription, p discount 30 gm elimite free shipping. Behavior system imbalance and instability are The goal of the system’s action is behavioral sys- not described explicitly but can be inferred from tem balance. For the nurse, the area of concern is a the following statement to be a malfunction of the behavioral system threatened by the loss of order behavioral system: and predictability through illness or the threat of illness. The goal of nurses’ action is to maintain or The subsystems and the system as a whole tend to be restore the individual’s behavioral system balance self-maintaining and self-perpetuating so long as con- ditions in the internal and external environment of and stability or to help the individual achieve a the system remain orderly and predictable, the condi- more optimal level of balance and functioning. She also identified are not met, malfunction becomes apparent in behav- questions to be asked when analyzing system func- ior that is in part disorganized, erratic, and dysfunc- tioning, and she provided diagnostic classifications tional. Illness or other sudden internal or external to delineate disturbances and guidelines for inter- environmental change is most frequently responsible ventions. The nurse also acts within and upon the ex- an adequate understanding of the potential for and ternal environment and the internal interactions of means to obtain a more optimal level of behavioral the subsystem to create change and restore stability. Structural and functional may train the client to cope with new stimuli and problems develop when the system is unable to encourage effective behaviors), stimulation (provi- meet its own functional requirements. As a result of sion of stimuli that brings forth new behaviors or the inability to meet functional requirements, increases behaviors, that provides motivation for a structural impairments may take place. In addition, particular behavior, and that provides opportuni- functional stress may be found as a result of struc- ties for appropriate behaviors), and protection tural damage or from the dysfunctional conse- (safeguarding from noxious stimuli, defending quences of the behavior. Other problems develop from unnecessary threats, and coping with a threat when the system’s control and regulatory mech- on the individual’s behalf). The model differentiates four diagnostic classifi- cations to delineate these disturbances. Disorders found between more than one subsystem Fundamental to any professional discipline is the are classified either as an incompatibility, which ex- development of a scientific body of knowledge that ists when the behaviors of two or more subsystems can be used to guide its practice. Nursing therapeutics deal with these three structure and rationale for activities; direction to areas. There are at least three types of interventions that the nurse can use Stevenson and Woods state: “Nursing science is the to bring about change. The nurse may attempt to domain of knowledge concerned with the adapta- repair damaged structural units by altering the in- tion of individuals and groups to actual or poten- dividual’s set and choice. The second would be for tial health problems, the environments that the nurse to impose regulatory and control meas- influence health in humans and the therapeutic in- ures. The nurse acts outside the patient environ- terventions that promote health and affect the con- ment to provide the conditions, resources, and sequences of illness” (1986, p. The linking of instrument behav- demonstrated the usefulness of Johnson’s model in iors to a more general attribute provided not only a clinical practice in a variety of ways. The majority an evidential basis for interpreting the process un- of the research focuses on clients’ functioning in derlying the instrument scores, but also a basis for terms of maintaining or restoring behavioral sys- inferring researchable implications of the scores tem balance, understanding the system and/or sub- from the broader network of the construct’s mean- systems by focusing on the basic sciences, or ing. Anayis Derdiarian’s research program in- found that changes in the aggressive/protective volves both the client and the nurse as agents of subsystem made both direct and indirect effects on action. Derdiarian’s early research tested an instru- changes in other subsystems (Derdiarian, 1990). She focused on of cancer patients (Derdiarian, 1983; Derdiarian & the nurses’ assessment of the patient using the Forsythe, 1983). The re- approach expanded the view of nursing knowledge sults demonstrated by the instrument possessed from exclusively client based to knowledge about content validity, strong internal consistency, and the context and practice of nursing that is model thus strong reliability. Derdiarian also found that a the Johnson model’s eight behavioral subsys- model-based, valid, and reliable instrument could tems. The study also served to further validate her improve the comprehensiveness and the quality of instrument. The measure Derdiarian’s body of work reflects the complex- can be taken as an indicator of the construct of “be- ity of nursing’s knowledge as well as the strategic havioral set. Her arti- work of relations that were tied to observables and cle (Derdiarian, 1991) demonstrated the clear rela- were therefore empirically testable. This validation tionship between Johnson’s theory and nursing study linked a particular measure, the Derdiarian practice. It provided identify the most common nursing diagnoses of evidence that the measure exhibited, at least in part, hospitalized geopsychiatric patients. They found the network of relations derived from the theory of that 30 percent of the diagnoses were related to the the construct. My goal was to determine the causes of instability within and between subsystems (e. My first study (Holaday, 1974) compared the achievement behavior of chronically ill and healthy children. The study showed that chronically ill children differed in attributional tendencies when compared with healthy chil- dren and showed that the response patterns differed within the chronically ill group when compared to certain dimensions (e. Males and children diagnosed at birth attributed both success and fail- ure to the presence or absence of ability and little to effort. The results indicated behavioral system imbalance and focused my attention on interventions directed toward set, choice, and action. The next series of studies used the concept of “behavioral set” and examined how mothers and their chron- ically ill infants interacted (Holaday, 1981, 1982, 1987). Patterns of maternal response provided information re- lated to the setting of the “set goal” or behavioral set; that is, the degree of proximity and speed of maternal response.
Some studies have suggested that a tendency toward somatization appears to be more common in individuals who have low socioeconomic discount 30 gm elimite otc, occupational discount elimite 30 gm, and educational status discount elimite 30 gm on-line. Any physical symptom for which there is no organic basis but for which evidence exists for the implication of psycho- logical factors. Impairment in social or occupational functioning because of preoccupation with physical complaints 10. Psychosexual dysfunction (impotence, dyspareunia [painful coitus], sexual indifference) 11. Excessive preoccupation with physical defect that is out of proportion to the actual condition Common Nursing Diagnoses and Interventions (Interventions are applicable to various health-care settings, such as inpatient and partial hospitalization, community outpatient clinic, home health, and private practice. Possible Etiologies (“related to”) [Severe level of anxiety, repressed] [Low self-esteem] [Unmet dependency needs] [Secondary gains from the sick role] Defining Characteristics (“evidenced by”) Verbal report of pain [in the absence of pathophysiological evidence] Reduced interaction with people Facial mask [of pain] Guarding behavior [Demanding behaviors] [Refuses to attend therapeutic activities because of pain] [History of seeking assistance from numerous health-care professionals] [Excessive use of analgesics, without relief of pain] Self-focusing Goals/Objectives Short-term Goal Within 2 weeks, client will verbalize understanding of correla- tion between pain and psychological problems. Long-term Goal By time of discharge from treatment, client will verbalize a noticeable, if not complete, relief from pain. Monitor physician’s ongoing assessments and laboratory re- ports to ascertain that organic pathology is clearly ruled out. Recognize and accept that the pain is real to the individual, even though no organic cause can be identified. Denying the client’s feelings is nontherapeutic and hinders the develop- ment of a trusting relationship. Identification of the precipitating stressor is important Somatoform Disorders ● 181 for assessment purposes. This information will be used to develop a plan for assisting the client to cope more adaptively. These distractors serve in a therapeutic man- ner as a transition from focus on self or physical manifes- tations to focus on unresolved psychological issues. Help client connect symptoms of pain to times of increased anxiety and to identify specific situa- tions that cause anxiety to rise. Verbalization of feelings in a nonthreatening environment facilitates expression and resolution of disturbing emotional issues. Explore ways to intervene as symptoms begin to intensify, so that pain does not become disabling (e. Posi- tive reinforcement enhances self-esteem and encourages repetition of desired behaviors. Client verbalizes that pain does not interfere with comple- tion of daily activities. Client verbalizes an understanding of the relationship between pain and emotional problems. Client demonstrates ability to intervene as anxiety rises, to prevent the onset or increase in severity of pain. Long-term Goal By time of discharge from treatment, client will demonstrate ability to cope with stress by means other than preoccupation with physical symptoms. Monitor physician’s ongoing assessments, laboratory reports, and other data to maintain assurance that possibility of organic pathology is clearly ruled out. Knowledge of these data is vital for the provision of adequate and appropriate client care. Recognize and accept that the physical complaint is indeed real to the individual, even though no organic cause can be identi- fied. Denial of the client’s feelings is nontherapeutic and in- terferes with establishment of a trusting relationship. Identify gains that the physical symptom is providing for the client: increased dependency, attention, distraction from other problems. These are important assessment data to be used in assisting the client with problem resolution. Failure to do this may cause client to become extremely anxious, with an increase in maladaptive behaviors. Explain to client that any new physical complaints will be referred to the physician, and give no further attention to them. Explain that attention will be withdrawn if rumination about physi- cal complaints begins. Help client observe that physical symptoms occur because of, or are exacerbated by, specific stressors. Help client identify ways to achieve recognition from oth- ers without resorting to physical symptoms. Positive rec- ognition from others enhances self-esteem and minimizes the need for attention through maladaptive behaviors. Discuss how interpersonal relationships are affected by client’s narcissistic behavior. These approaches decrease anxiety and increase self-esteem, which facilitate adaptive responses to stressful situations. Client is able to demonstrate techniques that may be used in response to stress to prevent the occurrence or exacerbation of physical symptoms. Client verbalizes an understanding of the relationship between emotional problems and physical symptoms. If there is actual change in structure or function, encourage client to progress through stages of grieving. Assess level of knowledge and provide information regarding normal griev- ing process and associated feelings. Knowledge of acceptable feelings facilitates progression through the grieving process. Use of touch may help him or her recognize acceptance of the individual by others and reduce fear of rejection because of changes in bodily structure or function. Self-care activities accomplished inde- pendently enhance self-esteem and also create the necessity for client to confront reality of his or her bodily condition.
Bio- feedback is often used together with other relaxation tech- niques such as deep breathing cheap 30gm elimite fast delivery, progressive relaxation buy elimite 30 gm fast delivery, and mental imagery 30gm elimite for sale. Assertive behavior increases self-esteem and the ability to develop satisfying interpersonal relationships. This is ac- complished through honesty, directness, appropriateness, and respecting one’s own rights, as well as the rights of others. Individuals develop patterns of responding in various ways, such as role modeling, by receiving positive or negative rein- forcement, or by conscious choice. These patterns can take the form of nonassertiveness, assertiveness, aggressiveness, or passive-aggressiveness. Nonassertive individuals seek to please others at the expense of denying their own basic human rights. Assertive individuals stand up for their own rights while protecting the rights of oth- ers. Those who respond aggressively defend their own rights by violating the basic rights of others. Individuals who respond in a passive-aggressive manner defend their own rights by expressing resistance to social and occupational demands. Some important behavioral considerations of assertive be- havior include eye contact, body posture, personal distance, physical contact, gestures, facial expression, voice, fluency, tim- ing, listening, thoughts, and content. Example: “I don’t want to go out with you tonight,” instead of “I can’t go out with you tonight. Example: Telephone salesperson: “I want to help you save money by changing long-distance services. Example: Male board member: “You made a real fool of yourself at the board meeting last night. Changing the focus of the communication from discussing the topic at hand to ana- lyzing what is actually going on in the interaction. Concurring with the critic’s argu- ment without becoming defensive and without agreeing to change. Putting off further discussion with an angry in- dividual until he or she is calmer. In cognitive therapy, the in- dividual is taught to control thought distortions that are consid- ered to be a factor in the development and maintenance of mood disorders. In the cognitive model, depression is characterized by a triad of negative distortions related to expectations of the environment, self, and future. The environment and activities within it are viewed as unsatisfying, the self is unrealistically devalued, and the future is perceived as hopeless. In the same model, mania is characterized by a positive cognitive triad—the self is seen as highly valued and powerful, experiences within the environment are viewed as overly positive, and the future is seen as one of unlimited opportunity. Therapy focuses on changing “automatic thoughts” that occur spontaneously and contribute to the distorted affect. Another technique involves evaluating what would most likely happen if the client’s automatic thoughts were true. He or she should be reassured that there are a number of techniques that may be used, and both therapist and client may explore these possibilities. Cognitive therapy has been shown to be an effective treatment for mood disor- ders, particularly in conjunction with psychopharmacological intervention. The current is sufficient to induce a grand mal seizure, from which the desired therapeutic effect is achieved. It is sometimes administered in conjunction with antidepressant medication, but most physicians prefer to perform this treat- ment only after an unsuccessful trial of drug therapy. There has been evidence, however, of its effectiveness in the treatment of acute schizophrenia, particularly if it is accompanied by cata- tonic or affective (depression or mania) symptomatology (Black & Andreasen, 2011). Other conditions, although not considered absolute contraindications, may render clients at high risk for the treatment. They are largely cardiovascular in nature and include myocardial infarction or cerebrovascular accident within the preceding 3 months, aortic or cerebral aneurysm, severe underlying hypertension, and congestive heart failure. It is impor- tant for the nurse to be present when the client awakens, to alleviate the fears that accompany this loss of memory. The major cause is cardiovascular complications, such as acute myocardial infarction or cardiac arrest. However, some clients have reported retrograde amnesia extending back to months before treatment. Although the potential for these effects appears to be mini- mal, the client must be made aware of the risks involved before consenting to treatment. Risk for aspiration related to altered level of consciousness immediately following treatment. Disturbed thought processes related to side effects of tempo- rary memory loss and confusion. Ensure that physician has obtained informed consent and that a signed permission form is on the chart. Prior to the treatment, client should void, dress in night clothes (or other loose clothing), and remove dentures and eyeglasses or contact lenses. Assist physician and/or anesthesiologist as necessary in the administration of intravenous medications. A short-acting anesthetic, such as methohexital sodium (Brevital sodium), is given along with the muscle relaxant succinylcholine chloride (Anectine).
List the average amount of sleep required for True False the following age groups buy elimite 30 gm line. Older adults: time order 30gm elimite amex, he/she will return to sleep again by starting at the point in the cycle where 3 cheap elimite 30gm with mastercard. Exercise that occurs within a 2-hour interval before normal bedtime stimulates sleep. The administration of a larger mid-afternoon dose of asthma medication may prevent i. True False Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins. Study Guide for Fundamentals of Nursing: The Art and Science of Nursing Care, 7th Edition. Maher, age 28, consumes four in a sleep history when a sleep disturbance is alcoholic drinks when watching television noted. After eliminating the alcohol from her diet, she complains of waking after a short period and not being able to fall back to sleep. Eichorn, age 45, has two teenage sons confirm that a patient is getting sufficient rest who are often out late at night. She cannot to provide energy for the day’s activities or val- get to sleep until they are both home idate the existence of a sleep disturbance that safely, and even then she continues to is decreasing the quantity or quality of sleep. Describe how you would prepare a restful environment for a home healthcare patient b. List three measures a nurse can take to help falling asleep, but the noise of the hospital alleviate a patient’s sleep problem. Loper, a 74-year-old patient in a long- ask a patient to assess for the following sleep term care facility, is bored during the day factors. Quality of sleep: that he is sleepy all the time but cannot sleep when he lies down after work. Number and duration of naps: Copyright © 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins. Study Guide for Fundamentals of Nursing: The Art and Science of Nursing Care, 7th Edition. Interview several friends or relatives to find out what they do to prepare for a restful night’s sleep. Nature of a sleep disturbance: man who has recently been admitted to a long-term care facility. Onset of a disturbance: don’t fall asleep until after midnight and then I’m up twice to go to the bathroom and have a lot of trouble falling back to sleep. Causes of a disturbance: ter has mentioned to the nurse that her father spends a lot of time napping during the day. What intellectual, technical, interpersonal, factors on the ward that would contribute to a and/or ethical/legal competencies are most patient’s sleep deficit. Develop a sleep teaching tool that explains the typical sleep patterns and requirements for patients of all ages (infants to older adults). What resources might be helpful for Include common factors that disrupt sleep pat- terns, total amount of sleep required, and pos- Mr. Interview individuals who have tried your interventions and evaluate the like- lihood that your teaching tool will resolve sleep problems. Study Guide for Fundamentals of Nursing: The Art and Science of Nursing Care, 7th Edition. I used to think my sleep habits were bad at school, but this is a Read the following patient care study and use hundred times worse because there never your nursing process skills to answer the seems to be time to crash. Identify pertinent patient data by placing a nurse, has been in her new position as a criti- single underline beneath the objective data in cal care staff nurse in a large tertiary-care med- the case study and a double underline beneath ical center for 3 months. Complete the Nursing Process Worksheet on of time for other things I want to do, but I’m page 223 to develop a three-part diagnostic not so sure anymore,” she says. Write down the patient and personal nursing it seems I’m always tired and all I think about strengths you hope to draw on as you assist all day long is how soon I can get back to bed. Worst of all, when I do finally get into bed, I often can’t fall asleep, especially if things have Patient strengths: been busy at work and someone ‘went bad. At that time, she “bounced into work” looking fresh each morning, and her features were always animated. Pretend that you are performing a nursing the “brightness” that was so characteristic assessment of this patient after the plan of of her earlier is strikingly absent. Study Guide for Fundamentals of Nursing: The Art and Science of Nursing Care, 7th Edition. For the purposes of this exercise, develop the one patient goal that demonstrates a direct resolution of the patient problem identified in the nursing diagnosis. Study Guide for Fundamentals of Nursing: The Art and Science of Nursing Care, 7th Edition. Somatic pain endings that are involved in fast-conducting, acute, well-localized pain include which of c. The highest level of integration of sensory which of the following facts about pain? A patient who recently underwent amputation patient to see whether the pain is manu- of a leg complains of pain in the amputated factured or psychogenic before starting part. The pain cannot exist because the leg has istence and nature of her pain, and pain been amputated.
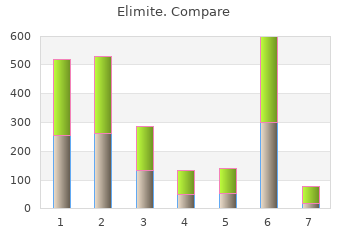
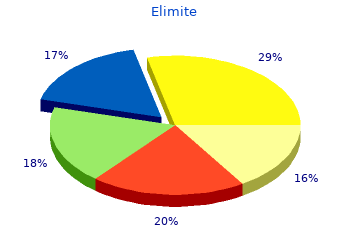
10 of 10 - Review by A. Frillock
Votes: 322 votes
Total customer reviews: 322