By Y. Ortega. University of Colorado, Denver. 2018.
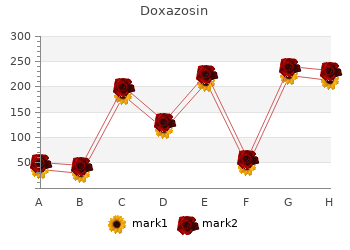
Nutrition is acknowledged to have a significant impact on optimal functioning of the immune response (Boyd et al doxazosin 1 mg cheap. Malnutrition is characterized by depletion of antioxidants generic 4 mg doxazosin overnight delivery, immune dysfunction cheap doxazosin 1 mg with amex, reduction of T lymphocytes and hormonal disturbances with increased cortisol levels in blood and saliva (Hughes et al. Periodontal infections may be adversely affected by malnutrition with alterations in the oral microbial flora as well as reductions in saliva production and its antibacterial components (Enwonwu, 1995). Studies linking nutritional status and periodontitis have largely focused on a number of micronutrients including the Ascorbic acid (vitamin C), vitamin B-complex, and calcium levels. Of the vitamins, ascorbic acid has received the majority of attention largely due to its historical association with scurvy, which has pronounced effects on the oral cavity (Fain et al 1998). Other forms of periodontal destruction have been noted with the 55 reduction of vitamin C intake. Initial studies on vitamin C deficiency in Guinea pigs were carried out by Glickman, (1948). Histology revealed that animals on a vitamin C deficient diet for 30 days developed deeper probing depths, edema and hemorrhage in the periodontal tissues. Lack of Vitamin C was proposed to cause a reduction in connective tissue, inflammatory cells, and inhibit fibroblast proliferation. A study conducted by Waerhaug, (1958) on vitamin C-deficient monkeys demonstrated increased osteoclastic activity leading to increased alveolar bone resorption. Studies showing positive associations with nutritional deficiencies and periodontal disease Author Study Type Nutrient Deficiency Results Glickman et al. Animal; Guinea Vitamin C (none-30 days) Increased periodontal 1948 Pig inflammation and destruction Vogel et al. Cross sectional, 35 Vitamin C (4 day diet analysis) Periodontitis patients had 1979 periodontitis significantly lower vit. Animals; Rats Calcium deficient Osteoporotic alveolar 1969 bone changes and reduction in periodontal ligament fibers Nishida et al. A four day diet analysis was conducted on a small sample of 35 patients (19 females 16 males) between 22 to 59 years old and presenting with generalized moderate to severe periodontitis. They calculated the amount of calories carbohydrates, fat, protein, sodium, calcium, phosphorus, thiamine, niacin, folic acid, fluoride, cholesterol, vitamins A, C, E, and B12 consumed by periodontitis subjects and compared these with 1,222 individuals of the general population without periodontitis. Results demonstrated significantly lower levels of riboflavin and vitamin C consumption by the periodontitis subjects compared to the general population but levels were above the recommended daily allowance. Interestingly, a large percentage of periodontitis subjects showed deficiency in calcium, magnesium, iron, vitamin E and folic acid. This study also found that intake of ascorbic acid in amounts larger than those recommended by the dietary standards does not seem to be associated with better periodontal health. Analysis of over 12,000 subjects using a 24-hour dietary recall but without information on supplement use was conducted to determine the effect of low vitamin C on periodontitis risk. Studies evaluating the role of vitamin C on periodontal status appear to indicate that a weak, but statistically significant effect may be present. In contrast, studies evaluating the effects of vitamin C supplementation on the response to periodontal therapy have largely failed to show any preventable benefit or strong association between such supplements and clinically relevant improvements in therapeutic results. The role of Vitamin C in protection from periodontitis may be related to antioxidant properties which can neutralize free radicals associated with increased oxidative stress in periodontitis subjects. Vitamin C has also been shown to suppress macrophage production of free radicals and is a primary cofactor in collagen synthesis as seen with scorbutic gingivitis an ulcerative condition of the gingival tissues under conditions of severe vitamin C deficiency (Fain et al. Although studies have not shown a clear relation between plasma ascorbate levels and inflammatory periodontitis, this epidemiologic evidence of vitamin C intake and periodontal disease, especially among smokers, may be of significance and warrant further prospective randomized controlled trials. Although oral manifestations are usually confined to the tongue (glossitis), Dreizen et al. The results showed that the animals developed a syndrome similar to pellagra as well as stomatitis. The stomatitis also produced a necrotizing gingivitis and periodontitis and an ulcerative and atrophic glossitis. Intuitively, more longitudinal studies are necessary to demonstrate prolonged affects of B-complex vitamins on gingival and periodontal health. Calcium and vitamin D deficiencies have been evaluated with respect to effects on the periodontal disease. Initial animal experiments involving rats found a reduction in the amount of periodontal ligament fibers along with reduction in alveolar bone density when animals where fed a diet deficient of calcium and vitamin D (Oliver et al. A longitudinal study demonstrated decreased tooth loss in subjects receiving supplemental calcium and vitamin D over 5 years (Krall et al. However 59 supplemental calcium did not have any effect on periodontal indices in patients with untreated periodontal disease (Uhrbom et al. The results of these studies seem to suggest that low dietary intake of calcium may result in increased risk for periodontal disease but that the effects of taking dietary supplemental calcium on arresting periodontal disease or as adjunctive aid in its treatment have not been thoroughly evaluated. The causes of this hyperinflammatory state are multifactorial and at present not fully understood. It is possible that dietary constituents or deficiencies may alter the hyperinflammatory phenotype causing a shift in the balance towards a proinflammatory or anti-inflammatory response. Not only are these free radicals released into the phagosome, but are also emitted into the extracellular matrix. It has been demonstrated that adult periodontitis patients generate higher levels of superoxide in their gingival fluid than healthy controls (Guarnieri et al. Antioxidants are molecules designed to limit oxidation reactions which transfer electrons to an oxidizing agent. Antioxidants interact with each other and with other metabolites either independently or synergistically (Knight et al. It is therefore 61 difficult to ascertain the exact role of individual antioxidants as each may depend on the function of other members of the group.
The basal sebocytes sit on a basal membrane at the outer limits of the lobes buy cheap doxazosin 1 mg line, and as cells move from the basal layer toward the lumen of the gland they synthesize lipids safe doxazosin 4 mg, which accumulate as intracellular lipid droplets buy doxazosin 4mg otc. As they synthesize lipid, the cells become larger, and the nucleus and other internal organ- elles are degraded. Ultimately, the entire mass of the cell is converted into a viscous liquid-phase lipid mixture. In most pilosebaceous units, sebum passes from the sebaceous gland into the hair follicle via the short sebaceous duct and outward onto the skin surface through the follicle. Generally, the hair follicle is large compared to the associated sebaceous gland; however, large sebaceous glands are associated with vellous hairs. These units are called sebaceous follicles and predominate on the forehead and cheeks. Distribution Pilosebaceous units are found over the entire surface of the skin except for the palmar and plantar regions (2). The density of follicles is greatest on the head, 45 46 Wertz and Michniak neck, and shoulders. In adults, the density of follicles on the scalp and face is in the range of 310 to 900 per square centimeter (1,3,4). On the torso and limbs the density of follicles is generally less than 100 per square centimeter (3). Large sebaceous glands are present in the submucosal connective tissue of the lip and buccal mucosa (5,6). Sebaceous glands in the oral mucosa often appear as slightly raised yellow spots, called Fordyce spots. Specialized sebaceous glands are also present on the edge of the eyelid (7) and the areolae of the nipples (3). Sebum Secretion Methods for Measurement Early attempts to measure sebum secretion rates involved removal of lipid from the skin surface, followed by protection of a defined area of skin for a standard time (8,9). At the end of the timed interval, lipids were collected by extraction and analyzed either gravimetrically or chromatographically. These extraction- based methods tended to remove sebum from the follicles as well as some of the epidermal lipid from the stratum corneum. Therefore, methods based on direct extraction invariably overestimated the amount of lipid on the skin surface. More recent investigations of sebum secretion have been based on adsorp- tion of sebum as it is secreted. With all three methods, the most frequent site of measure- ment has been the forehead, and the skin surface is depleted of sebum at the outset of measurement. With the cigarette paper method, the paper is delipidized by extraction with ethyl ether. After thorough drying, the paper is held in contact with the skin surface by means of a gauze strip. After a defined, standardized collection time, the paper is removed, and adsorbed lipids are extracted into ethyl ether and ana- lyzed. Total lipid can be determined by evaporating the solution onto a tared aluminum planchet or by thin-layer chromatography in conjunction with photo- densitometry (15). Although the cigarette paper method has been useful, it may overestimate sebum secretion because the paper tends to deplete sebum from the follicular reservoir in addition to that which would have been secreted in the absence of an adsorbent. The complications introduced by the follicular reservoir were most effec- tively addressed by the bentonite method (12), where bentonite gel is applied to the forehead 14 h before the start of the measurement period; the bentonite coat- ing is replaced after 6 h. At the beginning of the measurement period, two Sebum 47 small dacron disks are imbedded in freshly applied bentonite near the center of the depleted region. After 3 h, the disks are removed, and the lipids are extracted into ethyl ether and analyzed by quantitative thin-layer chromatography. This method yields the sustainable sebum secretion rate, which should reflect the rate at which sebum is synthesized. Although this method has been used in several studies of great importance (cited later in this chapter), it has not been widely used. This is at least in part because the suitability of bentonite for this application varies from one batch to another. Currently the most widely used method for studying sebum secretion is based on a porous polymeric tape called Sebutape, which is coated with a weak adhesive sufficient to hold it in contact with the skin. As sebum is secreted from the orifice of a follicle, it is adsorbed into the pores in the polymer and the appear- ance of the tape changes from opaque to transparent. Densitometric and com- puter-assisted image analysis methodology can yield information on the sebum secretion rate per unit area of skin or per follicle, as well as follicle density. A more extensive review of the above methods—as well as several variant methods based on the decrease in light scattering of a rough surface when it becomes coated with lipid—has recently been published (16). Hormonal Control Sebaceous glands are stimulated by androgenic hormones produced by the testes, ovaries, and adrenal glands (3,17,18). The ovaries also produce some testosterone, androstenediol, and dehydroepiandrosterone; however, the significance of these steroidal hor- mones in regulation of female sebaceous gland activity is uncertain. Dehydroepi- androsterone and dehydroepiandrosterone sulfate produced by the adrenal glands are the major circulating androgens in women and are also significant in men. In the sebocytes, the androgenic hormone binds to a cytosolic receptor, which then translocates to the nucleus and modulates gene expression (19–21). Variation with Age and Gender Sebaceous gland activity is high in utero, and this is responsible for production of the vernix caseosa, a coating of sebaceous lipid and exfoliated stratum corneum material that coats the newborn (22). By 1 year after birth, the sebum secretion rate is extremely low and remains so until the onset of puberty (23). At that time, the increased concentrations of androgenic hormones cause a rapid increase in sebum secretion rates.
There’s a significant cost to unskillfully managing stress order 4 mg doxazosin overnight delivery, which is a problem for at least 75 percent of the adults in the United States quality doxazosin 1mg. You can see how this could lead to exhaustion trusted 1mg doxazosin, a greater susceptibility to contagious illness, decreased sex drive, low blood pressure, and orthostatic hypotension (you can’t keep your blood pressure normal when you stand up, and feel like lying down again, literally and figuratively). Cortisol and Aging Women in their twenties are the hormonal gold standard, and under normal conditions, produce a tidy 15 to 25 mg of cortisol per day. In a survey of more than 300,000 Americans, those with the worst mental health scores were between ages thirty-five and fifty. High cortisol generates the long list of maladies associated with too much of this hormone. When we age, however, we don’t absorb cortisol into the cells the way we used to in our twenties and thirties (not to mention that high cortisol itself accelerates aging). These two imbalances—in the blood and in the cells— means that we feel tired (low cortisol) and wired (high cortisol). How High Cortisol Accelerates Aging Recall that cortisol’s main job is to normalize your blood- sugar levels. This may lead to prediabetes (as measured by a fasting glucose level between 100 and 125 mg/dL) or diabetes (fasting glucose > 125). The marathon runner has far higher cortisol levels from running, gets more injuries, and ages faster. Not only that, prolonged elevation of cortisol causes a domino effect: when your adrenals are monomaniacally producing cortisol, the rest of the hormone cascade falls into neglect. Here’s what concerns me most: extensive research demonstrates that prolonged exposure to high cortisol constricts blood flow to the brain. That adversely affects brain function, decreases your emotional intelligence, and accelerates age-related cognitive function. Yes, Alzheimer’s disease becomes established more than thirty years prior to symptoms. Ideally we make a lot in the morning, less during the day, very little at bedtime, and a minimal amount while we sleep. Referred to as diurnal variation —diurnal simply means a recognizable daily cycle, similar to how a flower opens and closes during a twenty- four-hour cycle—the process can be documented in a “diurnal cortisol” measurement at four points between about six a. It also sets up one of your most important circadian rhythms, another crucial aspect of hormonal control. Operating on a twenty- four-hour cycle, circadian rhythms establish your biochemical and physiological peaks and valleys, almost like a tide within the body. When the cortisol tide is out, around midnight, and your cortisol is at its lowest, your cells perform their greatest repair and healing. If your cortisol is still high at night, your body can’t do the repair work it needs. That’s no good: when you are most in need of rest, the high cortisol makes you feel you don’t need it—which only depletes your adrenals further, because your adrenals heal at night. Furthermore, depleting your adrenals will cause you to start running low on important feel-good neurotransmitters, including serotonin, dopamine, norepinephrine, and epinephrine. In addition, nighttime is when your hormones get a chance to harmonize and resync with one another. Melatonin and growth hormone, for instance, which help you fall asleep and stay asleep, are mainly secreted at night. If you are low in one or both, your cortisol may become inappropriately high at night; over time, the lack of sleep may make it harder to sleep because of higher cortisol. In older, traditional cultures, you’d start to unwind with the loss of light as the sun went down. Artificial light allows us to catch up on e-mail, finally listen to that webinar, sign our kid’s field-trip permission slip, and order a birthday gift, all while getting dinner together. With high evening cortisol, it’s no wonder you have trouble falling asleep, staying asleep, or sleeping deeply. I’ve had hundreds of women tell me they simply can’t understand why they feel tired in the morning after they’ve slept eight hours. More times than not, they’re checking e-mail, reviewing the next day’s to-do list, or catching up on a crime show. It doesn’t take a Harvard-educated gynecologist to understand why these women can’t get some decent shut-eye. Most folks with symptoms of overwhelming stress have low cortisol in the morning and high cortisol at night—the opposite of what it’s supposed to be. What you want is that diurnal variation: a steep, downward slope to your cortisol levels. Find Out If You Have High Cortisol In mainstream medicine, you don’t often find a doctor who is interested in checking your cortisol levels unless you’re a textbook case of Cushing’s syndrome, a rare cause of excess cortisol found in just one out of 500,000 people. People with Cushing’s have a long list of symptoms, some of which overlap with those in my questionnaire, but most of which are more extreme. Most doctors will screen for this with a urine cortisol test, but even the best screening test for Cushing’s is subject to debate. Another reason to test your cortisol is a relatively new hormonal condition that is garnering more attention among conventional doctors: subclinical hypercortisolism, which lacks clear diagnostic criteria. The rate of hypertension, or high blood pressure, is 48 to 92 percent—a consequence of excess cortisol. But there’s no clear diagnostic criteria for how high is too high when it comes to cortisol, which makes distinguishing between stress- related excess cortisol and Cushing’s syndrome difficult. If you find you have five or more of the problems in the questionnaires of Part A and/or Part B of chapter 1, I recommend starting The Gottfried Protocol with the lifestyle adjustments, but test before going further and trying the botanical or bioidentical therapies.
Instead cheap doxazosin 1 mg online, as new parents will testify safe 1mg doxazosin, young babies have a sleep cycle that lasts only around 3±6 h buy doxazosin 2mg lowest price. The functions of these different phases of sleep are not at all clear but chronic sleep deprivation does eventually lead to death. This would be consistent with its greater occurrence during the early stages of the sleep cycle when hormone secretion supports anabolic metabolism. These cells generate sufficient extracellular current for it to reach, and be recorded from, the cranium and scalp. However, the rhythm and appearance of spindles in earlier phases of the sleep cycle do depend on links with the thalamus (see Steriade 1999). Unlike stimulation of the specific sensory relay nuclei in the thalamus, which only affects neurons in the appropriate sensory areas of the cortex, the non- specific nuclei can produce responses throughout the cortex and may not only control, but also generate, cortical activity. Maintenance of these frequencies relies on the degree of depolarisation of the thalamic neurons (Jahnsen and Llinas 1985) and this, in turn, depends on the nature and intensity of their afferent inputs. In fact, it has been suggested that the stronger and clearer these oscillations become, the more likely it is that there will be loss of consciousness. Apart from neuronal inputs originating in the cortex, thalamic afferents (see Fig. Because these neurons are themselves activated by sensory inputs transmitted along the spinothalamic tract, this provides one way in which sensory stimuli can influence cortical activity generally, as well as specifically. As described below, these seem to be particularly important and probably disrupt the thalamo-cortical synchrony. Conversely, transection that separated the entire brain, including the brainstem, from the spinal cord (at the level of Cl) caused continuous arousal. Indeed, this is another way in which sensory stimuli can affect our state of arousal (Fig. It is activated by impulses in collaterals of the spinothalamic sensory pathway running to specific thalamic nuclei (SpThNc) and in turn activates much of the cortex, partly through the non-specific thalamic nuclei (NspThNc), which also receive inputs from SpThNc and also via the nucleus basalis (NcB). Thus, not only will the sensory cortex be more responsive to any primary sensory input it receives, but its activation keeps us alert. Together, these links could help to ensure smooth progression from one state of arousal to another. It is important to emphasise that a lesion of the reticular system disrupts a number of afferent inputs to the cortex. When the ascending inputs from these neurons are destroyed, sleep is passive and not at all like natural sleep which, as detailed above, has distinct phases and depends on brainstem influences on cortical function. How these different neurotransmitters might influence sleep and arousal will be considered next. These neurons innervate the cortex more than the thalamus and their possible roles will be considered in the following sections. This material draws on studies designed to show:which neurotransmitters are associated with those brain structures concerned with sleep and waking; how their function may change during the cycle; to what extent pharmacological manipulation of their activity influences the cycle; and how drugs which modify our state of arousal affect neurotransmitters. Yet antimuscarinic drugs do not have any marked sedative effects on behavioural arousal. One group lies rostrally in the basal forebrain, within the nucleus basalis, medial septum and diagonal band. The nucleus basalis, which sends diffuse projections to the cortex and hippocampus, has also been linked with memory function (Chapter 18). It innervates the non-specific thalamic nuclei as well as some more specific ones like the lateral geniculate nucleus (visual pathway), the pontine reticular formation and occipital cortex. The activity of histamine-releasing neurons increases with arousal and diminishes during sleep. Finally, other effects of histamine that could contribute to increased arousal are increasing the activity of excitatory cholinergic neurons in the basal forebrain and inhibition of neurons in the hypothalamic preoptic area which promote sleep. A much higher profile has recently been claimed for histamine in the control of circadian rhythm (see Jacobs, Yamatodani and Timmerman 2000). When injected intracerebroventricularly in rats it appears to alter locomotor and drinking rhythms in a somewhat complex manner depending on when it is given in the light±dark cycle, being most active when the animals are in constant darkness. Some of the effects can also be mimicked by increasing the amount of endogenous histamine released with the H3 autoreceptor antagonist thioperamine. Whether this is so remains to be seen for, despite the sedative effects of some H1 antagonists, rhythm changes have not been reported with their long-term clinical use. Because a reduction in the activity of noradrenergic neurons precedes the onset of sleep, this change in activity is thought to have a permissive role in sleep induction. How all these actions of noradrenaline are manifest is not clear and, unfortunately, most experiments in this area have been carried out on anaesthetised animals which, arguably, are not ideal for investigating mechanisms underlying arousal! These changes, which are thought to be mediated by activation of b-adrenoceptors, suggest that noradrenaline increases cholinergic influences on arousal, in the nucleus basalis, at least (Cape and Jones 1998). However, a fairly common side-effect of b-adrenoceptor antagonists, used clinically to relieve hypertension, is sleep disturbance which is expressed as nightmares, insomnia and increased waking. It has even been suggested that b-blockers disrupt sleep patterns by inhibiting melatonin synthesis and release, but this is controversial. Since their activation of presynaptic a2-autoreceptors will reduce noradrenergic transmission, by depressing the firing of neurons in the locus coeruleus and release of noradrenaline from their terminals, this action is entirely consistent with the proposal that increased noradrenergic transmission increases arousal. Although this presynaptic action of a2-agonists would explain their sedative effects it must be borne in mind that many a2-adrenoceptors in the brain are in fact postsynaptic. Their role (if any) in sedation is unclear but it must be inferred that, if they make any contribution to sedation, then either a specific brain region or a specific a2-adrenoceptor subtype is involved. Another possible confounding factor is that many a2-adrenoceptor ligands have an imidazoline structure (see Chapter 8) and the recently discovered imidazoline receptors are also thought to influence the sleep cycle and arousal.
10 of 10 - Review by Y. Ortega
Votes: 131 votes
Total customer reviews: 131